Colorectal Cancer
Colorectal cancer is the third commonest cancer in Hong Kong. In 2022, there were 5 190 new cases, contributing to 14.7% of all new cancer cases in Hong Kong. Of these, 2 928 were male and 2 262 were female.
In 2022, the crude annual incidence rate of colorectal cancer was 71 per 100 000 Hong Kong population. The median age at diagnosis for males was 69 years and that for females was 69 years. The age-specific incidence rates increased significantly from age 50 onwards. Colorectal cancer is more common among males, reflected by the male to female ratio of about 1.3 to 1 in 2022.
Colorectal cancer is the second leading cause of cancer deaths in Hong Kong. In 2022, a total of 2 270 people died from this cancer, accounting for 15.4% of all cancer deaths.
Colorectal cancer, if detected and treated early, is highly curable. Overall, the five-year relative survival rate was 58.2% for all stages combined. The rates were high for stage I (95.7%) and stage II (87.3%). It dropped to 68.7% for stage III and further declined to 9.3% for stage IV. Understanding its symptoms and causes can allow early detection and treatment of colorectal cancer. In addition, knowing more about its treatments, nursing and caring techniques can facilitate early recovery of the colorectal cancer and reduce the risk of relapse.
What is Colorectal Cancer?
Large bowel is the lower part of the digestive system, consisting the colon and rectum. Sometimes, abnormal cells will emerge on the bowel wall, growing into polyps, ulcers or other forms of mass. Most of the colorectal polyps are benign, but a small portion of them may develop into malignant tumours, becoming colorectal cancer.
Who have higher chance of having Colorectal Cancer?
Risk factors for colorectal cancer include low fibre intake, high consumption of red meat and processed meat, lack of physical activity, obesity, alcohol consumption and smoking. Individuals with the following risk factors are more prone to developing colorectal cancer:
- Having hereditary bowel diseases, e.g. familial adenomatous polyposis (“FAP”) or Lynch Syndrome;
- Persistent inflammation of the bowel, e.g. ulcerative colitis;
- History of colonic polyps; and
- Family history of colorectal cancer, particularly in first-degree relatives (i.e. parents, siblings or children).
What are the symptoms of Colorectal Cancer?
Early colorectal cancer may have no symptoms. Common signs and symptoms of colorectal cancer include:
- Bloody or stained stool, black stool, stools with mucus, or rectal bleeding;
- Change in bowel habits (persistent constipation or diarrhea), change in the shape of the stool (thin strip), feeling of incomplete bowel emptying;
- Unexplained weight loss;
- Lower abdominal pain (distended abdomen or colicky abdominal pain);
- Symptoms of anemia: cold hands and feet, fatigue, palpitation, shortness of breath, pallor, dizziness.
Prevention
Many of the risk factors for colorectal cancer (CRC) include low fibre intake, high consumption of red meat and processed meat, lack of physical activity, obesity, alcohol consumption and smoking.
Individuals with the following risk factors are also at increased risk of CRC–
- Some hereditary bowel diseases, e.g. familial adenomatous polyposis (“FAP”) or Lynch Syndrome;
- A long history of inflammation of the bowel, e.g. ulcerative colitis;
- History of colonic polyps; and
- Family history of CRC, particularly in first-degree relatives (i.e. parents, siblings or children).
By adopting healthy lifestyle, one eat more food rich in fibre, eat less red meat and processed meat, have regular physical activities, maintain a healthy body weight and waist circumference, and abstain from drinking alcohol and smoking to prevent or reduce the risk of getting CRC.
Screening
Asymptomatic individuals at average risk
CEWG recommends that people at average risk aged between 50 and 75 should consult their doctors to consider one of the following screening methods –
- Annual or biennial faecal occult blood test (“FOBT”); or
- Sigmoidoscopy every 5 years; or
- Colonoscopy every 10 years.
Increased risk individuals
- For carriers of mutated gene of Lynch Syndrome, it is recommended that screening for CRC by colonoscopy every 1 to 2 years from age 25 onwards.
- For carriers of mutated gene of FAP, it is recommended screening by sigmoidoscopy every 2 years from age 12.
- For individuals with one first-degree relative diagnosed with CRC at or below 60 years of age, or more than one first-degree relatives with CRC irrespective of age at diagnosis, colonoscopy should be performed every 5 years beginning at the age of 40 or ten years prior to the age at diagnosis of the youngest affected relative, but not earlier than 12 years of age. As an alternative, the concerned individuals may consider FIT every one or two years after understanding the pros and cons of FIT as compared with colonoscopy.
* Recommendation on genetic testing for CRC: For family members of CRC patients with identifiable genetic mutations, two-tier screening by genetic testing followed by endoscopic examination can be offered to reduce the number of unnecessary investigations, as well as to reduce the risk of potential complications.
Colorectal Cancer Screening Programme
Regularised by the Government in August 2018, the Colorectal Cancer Screening Programme (“CRCSP”) aims to heavily subsidise asymptomatic Hong Kong residents to undergo screening tests in three phases. The first and second phases cover people aged 61 to 75 and those aged 56 to 75 respectively, while the coverage further extended to cover those aged 50 to 75 starting on 1 January 2020. Participants would first receive subsidised Faecal Immunochemical Test (“FIT”) screening from enrolled primary care doctor (“PCD”) and if the FIT result is positive, the participant will be referred to see an enrolled colonoscopy specialist to receive a colonoscopy examination subsidised by the Government.
For more information, please visit the Department of Health “Colorectal Cancer Screening Programme” 's website.
How to investigate and make diagnosis for Colorectal Cancer?
High-risk individuals and people with the above-mentioned symptoms should consult doctors and arrange investigation as soon as possible. Detection of colorectal cancer at early stages can increase the chance of cure. Investigations include:
-
anchor
Sigmoidoscopy & colonoscopy
Colonoscopy is currently the best method to examine the lower digestive tract. By means of a flexible video-endoscope, the entire length of the colon as well as the terminal portion of the small bowel could be examined. The procedure generally lasts for 10 to 45 minutes. Sigmoidoscopy is used to examine the rectum and the distal part of the sigmoid colon.
Colonoscopy is not only useful for diagnosis, but also therapeutic. With different accessory equipment, it can perform biopsy and deliver targeted procedures such as removal of polyp.
Risk and complications
Minor discomfort, including abdominal pain and distension, may occur. Major complications such as perforation, bleeding, heart and lung complications, infection or acute intestinal obstruction are uncommon, with a risk of less than 1%. Patients should seek immediate advice from doctors if they experience abdominal pain or note blood in stools after the procedure.
-
anchor
Barium enema examination
Barium enema is a special x-ray procedure used for study of large intestine. Barium will be delivered through a well-lubricated tube into the rectum by a radiologist. Liquid barium acts as a contrast to highlight specific areas on the large bowel wall. The flow of the barium will be shown on an x-ray fluoroscope screen to indicate any abnormalities of the inner bowel wall.
-
anchor
Rectal examination
Physician will insert a gloved and lubricated finger into the rectum through the anus and palpates for any abnormal lesions or tumours.
-
anchor
Fecal Occult Blood Test
Bleeding in the bowel may not be visible. Fecal Occult Blood Test checks for hidden blood in the stool. If the test result is positive, further examination is needed such as colonoscopy or barium enema examination.
-
anchor
Blood Test
Blood markers such as carcinoembryonic antigen (CEA) have been found to be elevated in some patients with colorectal cancers. However, such marker has limited sensitivity and specificity, and the role is mainly for disease monitoring and prognosis.
If a tumour is found, doctors may arrange computed tomography tests and other imaging studies.
What is the treatment for Colorectal Cancer?
The major treatment modalities for colorectal cancer include:
-
anchor
Surgery
Surgical removal of tumour is the primary treatment for colorectal cancer. It can cure early-stage colorectal cancer and a few advanced cases which have metastasized to liver or lung. In recent year, some cases have been treated by minimally invasive surgery which not only speeds up rehabilitation but also greatly reduces the risk of complications. However, it is not applicable for every patient. For rectal cancer, total mesorectal resection is advocated to improve the chance of cure, but temporary or permanent stoma may be necessary in individual patients.
-
anchor
Adjuvant therapy
Adjuvant therapy can reduce the chance of relapse and improve survival rates, especially for those who have a higher risk of relapse after radical surgery for colorectal cancer. Adjuvant treatment includes radiation therapy and chemotherapy. Radiotherapy uses of high-energy radiation to kill cancer cells. It is mainly used in rectal cancer patients. Chemotherapy is the use of anti-cancer drugs to kill cancer cells. These treatments are usually given after the radical surgery. Selected patients may require perioperative chemoradiotherapy, which aims to reduce the chance of local recurrence and improve the overall survival rate of patients.
Who needs adjuvant therapy?
- Adjuvant treatment may be considered for Stage II colorectal cancer patients with high-risk features.
- Adjuvant treatment is generally recommended in Stage III colorectal cancer patients.
- For stage IV colorectal cancer patients, adjuvant treatment is considered only if all of the detected tumours including the primary tumour and metastatic lesions can be or have been completely resected.
-
anchor
Palliative treatment
Depending on the patients’ condition and the impacts of the cancer on the patients, individual patients with metastatic colorectal cancer may require palliative chemotherapy or radiotherapy to prolong their survival and relieve their sufferings. Targeted therapy and chemotherapy drugs may be used together to enhance the efficacy of treatment, taking into account the genetic mutation of the cancer cell.
What are the complications caused by Colorectal Cancer and its related investigations and treatments?
Colorectal cancer itself can cause intestinal obstruction, perforation of bowel, etc. Some colorectal cancer patients will suffer from malnutrition and anemia. Patients with hypertension, diabetes mellitus, coronary heart disease, and other chronic diseases should take more awareness.
-
Investigation
Patients who have undergone endoscopic therapy, such as polypectomy (removal of polyps), endoscopic hemostasis, expansion and stent placement might have a higher risk of serious complications such as intestinal obstruction and bleeding.
-
Surgery
Patients treated by surgery may have peritonitis and sepsis if their surgical wound is not healed well. Patients may also have colitis or urinary dysfunction after surgery. However, it is worth noting that the more commonly used minimally surgery for bowel cancer has greatly reduced the risk of surgical complications in recent years.
-
Chemotherapy
Common side effects of chemotherapy include fatigue, increased chance of infection or bleeding, loss of appetite, nausea and vomiting, hair loss, diarrhea, numbness of limbs. If patients experience these side effects, doctors will prescribe drugs according to the patients’ condition to relieve their symptoms.
-
Radiotherapy
Common side effects of radiotherapy include fatigue, nausea, skin reaction in the irradiated area, abdominal pain, diarrhea, painful bowel opening, urinary frequency or pain. Women may have vaginal discharge, itching and pain. If patients experience these symptoms, doctors will prescribe drugs according to the patients’ physical condition.
How to take care of Colorectal Cancer patient?
There are a lot of things to take care during the recovery process. Better understanding will help patients face the disease with a positive attitude.
-
Regular follow-up
Patients' condition, treatment and clinical features are different. Doctors would discuss with the patient, closely monitor patient' s recovery, review and assess follow-up treatments and propose consultation arrangements base on individual needs.
Regular follow-up helps pick up recurrence of the tumour or new tumours, ensures timely treatment as well as minimizing complications. Getting treatment early improves patients’ chance of cure.
-
Stoma
Patients who have the tumour in the lower rectum may have temporary and permanent stoma. Stoma Nurses will assist patients to choose the stoma appliances and empower patients the proper usage of stoma appliances and stoma care.
-
Diet
Patients are suggested to avoid eating food items that are difficult to digest such as fatty food and those may irritate the bowel e.g. curry or spicy food.
Colonoscopy / Sigmoidoscopy and Polypectomy
-
Introduction
Colonoscopy is currently the best method to examine the lower digestive tract. By means of a flexible video-endoscope, the entire length of the colon as well as the terminal portion of the small bowel (if indicated) can be examined. Colonoscopy is often the investigation of choice in patients with suspected diseases of the colon or terminal ileum such as colorectal cancer, or in the presence of rectal bleeding, occult blood in stool, change of bowel habit, chronic diarrhoea, constipation, and difficulty in defecation. Colonoscopy is not only useful in making a diagnosis; with the use of different accessory tools, endoscopist can also perform biopsy and deliver targeted therapies such as removal of polyp.
-
The procedure
Colonoscopy and polypectomy is usually performed in the Endoscopy Unit, patient will be put in a lateral position with the thigh and leg flexed.
Prior to the procedure, intravenous sedation will be administered to the patient to alleviate patient anxiety and discomfort related to the procedure. Lubricant will then be applied to the anal region. A flexible colonoscope with a diameter of around 1.5cm will then be introduced by the endoscopist through the anus to examine the colon. Though under sedation, patients may still be conscious during the procedure. In general, the procedure will last for 10 - 45 minutes. In complex cases that require additional therapies, the examination time will be prolonged. Patients’ co-operation with medical staff will help shorten the examination time.
If a small polypoid growth (<2cm) known as polyp is found, it will be removed by polypectomy. While removing polyps, the patient will not feel pain. Most polyps are benign. Only a handful of polyps will develop into cancer.
-
Risk and complication
Colonoscopy and polypectomy are generally safe, but the following complications may also occur.
Minor discomfort, including abdominal pain and distension, is common. Major complications, including perforation, bleeding, cardiopulmonary complication, infection or acute intestinal obstruction may happen. In general, the risk of major complications is less than 1%, but it varies depending on patients’ conditions and the complexity of the diagnostic and therapeutic methods used. Complication rate will be higher in cases that require therapeutic procedures including polypectomy, endoscopic haemostasis, dilatation or stenting. When major complications arise, emergency surgical treatment may be needed and mortality may happen. Patients should consult the attending physicians for the detail of the endoscopic procedures.
-
Preparation before the procedure
Patients should consume a low-residue diet for 3 days prior to the procedure. Iron preparation should be stopped at least 3-4 days before colonoscopy. Before the examination, patients will be instructed to drink liquid purgatives to wash out faeces from the colon to allow a clear endoscopic inspection of the colonic wall. Patients need to follow the instruction closely otherwise the examination may be failed due to retained faeces. Patients should inform medical staff of any major medical problems including diabetes, hypertension, valvular heart diseases and pregnancy and continue their medications as instructed. Patients should also provide information concerning the current medications used especially antiplatelet and anticoagulation drugs and any allergic history. Patients should avoid driving to attend the out-patient procedure and also avoid smoking, alcohol drinking and taking sedatives before the procedure. Elderly patients and those with difficulty in walking should be accompanied by a family member.
-
After the procedure
Patients should resume oral intake only after the effect of anaesthetic or sedative has worn off. If intravenous sedation is used, patients should avoid operating heavy machinery, signing legal documents or driving for the rest of the day. Patients are advised to enquire about the examination results and date of follow-up after the examination. Patients should follow the instruction given by the medical staff in completing the drug treatment.
-
Follow up
Patients can contact the endoscopy unit for any discomfort after the procedure, or if the patients have any question about the examination result and drug treatment. However, if serious events develop, such as passage of large amount of blood, severe abdominal pain, etc. patients should seek medical advice at the nearest Accident and Emergency Department.
-
Colon assessment public-private partnership programme (Colon PPP)
To cater for the growing demand for colon assessment, the Hospital Authority (HA) has launched the Colon Assessment Public-Private Partnership Programme to provide subsidy to eligible patients to receive related services from private specialists. By utilizing the service capacity in private sector, the Programme offers choices to patients so that they can receive colonoscopy and appropriate treatment as early as possible.
Under the Programme, patients can choose one participating private specialist from the list who will provide clinical assessment, colonoscopy procedure and explanation of results. For patient requiring biopsy and /or polypectomy, tissue specimen will be sent by the performing private specialist for histopathology examination. The private specialist will also discuss further treatment plan with the patient if appropriate.
The HA will offer a one-off fixed subsidy of $6,800 (without polypectomy) or $7,500 (with polypectomy) to each patient. Patient will only need to bear a minimum co-payment of $1,000. An additional fee of up to $1,000 may be charged by the private specialist and the fees are clearly stated in the HA list of Specialists for patients to select. Participating patients who are eligible for a waiver under the criteria set out in the Programme can select enrolled private specialist offering no co-payment, while the co-payment amount of HK$1,000 will be borne by HA.
Subject to the availability of Programme quota, the HA has started invitation to patients in December 2016. Eligible patients include those who are currently on the waiting list for colonoscopy in public hospitals, classified as stable cases, and fit for home bowel preparation and colonoscopy under ambulatory setting. The Programme office issues invitation letters to patients in batches according to patients’ registered waiting time and clinical condition, and patients do not need to apply by themselves. Invited patients will then attend designated HA clinics to undergo assessment and submit enrollment forms. Patients also need to register for the Electronic Health Record Sharing System so that patients’ medical records and investigation results can be shared between the HA and private doctors.
For details, please refer to the HA website.
-
Remarks
For further information please contact your doctor.
Barium Enema Examination
-
Purpose
Suspected pathology in the large bowel.
-
Bowel preparation
The referring clinician will decide on one of the following preparation:
-
Oral bowel cleansing regimen:
Administer (Klean Prep or equivalent) one day before examination, according to the instruction sheet attached.
-
Rectal washout:
- Take 2 tablets of Dulcolax on the evening before examination.
- Cleansing enema should be performed 3 hours before the examination until the returning fluid is clear.
- After completion of cleansing enema, an 1-2 hours interval is required to allow water reabsorption within the bowel prior to the examination.
-
Oral bowel cleansing regimen:
-
Preparation before the procedure
The diagnostic accuracy of the examination depends to a large extent on the thoroughness of the bowel preparation.
- Maintain a low residual diet (i.e. one restricted to bread, potatoes, rice and other starchy foods, but no vegetables or fruits) for at least 48 hours prior to examination.
- Fluid diet 24 hours before examination.
- Omit the breakfast on morning of examination.
Note
- Please inform medical staff before the examination if you are or think you may be pregnant.
- For diabetic patient on drug - consult clinician concerned for the adjustment of insulin dosage if necessary.
-
The procedure
The examination is performed by a radiologist and it usually takes about 1 hour to complete. During the examination, contrast medium (containing barium compounds and air) is introduced into the large bowel via a rectal catheter under fluoroscopic guidance. A series of X-rays are then taken. Patient may experience abdominal distension and discomfort during the introduction of air and contrast medium. The discomfort will subside after the examination. Inform the radiologist as soon as possible if patient feel any pain. Patient should follow the instructions of the staff during the examination as various positions may be adopted to facilitate the flow of contrast media. Intravenous injection may be necessary to relax the large bowel.
-
After the procedure
Eat or drink as usual after the examination. Suggest increase fluid intake if not contraindicated. Stool will appear white in color for a few days.
-
Complications
Complications may occur only in patients with critical bowel lesions and the incidence is very low, such as:
- Perforation of bowel.
- Venous intravasation of contrast.
-
Remarks
For further information please contact your doctor.
Laparoscopic Colorectal Resection
-
Introduction
Intestine consists of small and large intestine (including ascending, transverse, descending and sigmoid colon and rectum). Large intestine is mainly responsible for water absorption and formation of solid stool which is stored in rectum and then passed out in anus.
Laparoscopic colorectal resection is a major operation in which part or whole of the colon or rectum is removed with the use of laparoscopic technique. It is a minimally invasive procedure, which smaller incisions are made, with less postoperative pain and associated complications, and earlier return of bowel function.
-
The procedure
- The operation is performed under general anaesthesia.
- Small incisions are made over the abdomen for insertion of laparoscope and instruments.
- Carbon dioxide is insufflated into the abdominal cavity.
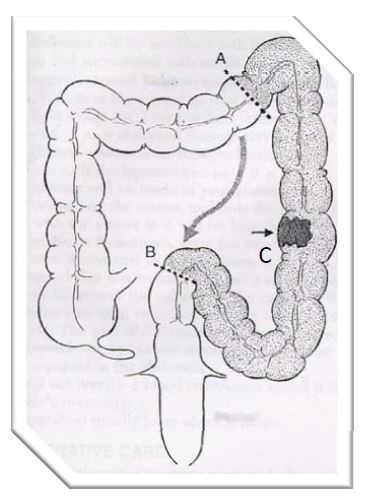
- Surgeon localizes the tumour(C) and excises the diseased segment of colon (A to B) using laparoscopic instruments (please refer to the diagram below for the position of tumour and colon segment).
- The remaining ends of bowel are usually rejoined when it is appropriate. Otherwise, a stoma may be performed as part of the operation, either temporarily or definitively.
- Depending on the nature of the disease and individual anatomy, it may be impossible or unsafe to proceed further with laparoscopic technique; the operation will then have to be converted to conventional open surgery.
-
Risk and complication
Anaesthesia related complications
- Cardiovascular complications: acute myocardial infarction, cerebral accidents, deep vein thrombosis, massive pulmonary embolism, etc.
- Respiratory complications: atelectasis, pneumonia, asthmatic attack, exacerbation of chronic obstructive airway disease, etc.
- Allergic reaction and anaphylactic shock.
Procedure related complications (Item 1-3: may require further major operation and are associated with an overall mortality of up to 5%)
- Complications related to bowel preparation (renal failure/electrolyte disturbance).
- Surgical emphysema and incisional hernia.
- Damage to spleen in case of splenic flexure mobilization.
- Injuries to the urinary bladder and ureter.
- Anastomotic bleeding, leakage or disruption (3-10%), leading to reoperation, stoma and anastomotic stricture.
- Intra-abdominal bleeding and collection.
- Bladder dysfunction – 20%; temporary in most cases (in rectal cancer surgery), urinary tract infection.
- Damage by trocars: urinary bladder, gastrointestinal tract or vessels.
- Transient faecal incontinence, intestinal obstruction (prolonged ileus/adhesive obstruction).
- Sexual dysfunction, impotence (30-40%) (in rectal cancer surgery).
- Wound complications: Infection, scar problems (hypertrophic scar, Keloid).
- Fatal air-embolism.
- Port site recurrence (local or systemic or both).
- Stoma complication: Necrosis, stenosis, bleeding, retraction, prolapse, parastomal hernia, high output and skin irritation.
-
Preparation before the procedure
- Pre-operative interview with doctor in charge on the diagnosis, option of management, nature of operation and possible risks. Completed the inform consent form.
- Pre-operative work up: physical examination, blood tests, chest X ray and electrocardiogram (ECG).
-
Bowel preparation:
- Low residue diet 3 days before operation, avoiding high roughage food such as vegetables, fruits and cereals.
- Fluid/congee diet 2 days before operation.
- Bowel cleansing agent may be prescribed on the day before operation; clear fluid (non-dairy products) is allowed.
- Pre-operative anesthetic assessment.
- Shaving of appropriate operative site and bathing.
- Keep fast for 6 hours before operation to avoid risk of aspiration.
- Change to operation room uniform before transferred to operating room.
- Urinary catherization may be required, otherwise empty bladder before surgery.
- May need pre-medications and intravenous drip.
- Antibiotics prophylaxis or treatment may be required.
- Patient should Inform doctors about drug allergy, regular medications or other medical conditions.
-
After the procedure
Usually after operation, patient may feel mild throat discomfort or pain because of intubation. Mild discomfort or pain over abdomen, shoulder or neck is common because of gas insufflations. Inform nurses or doctor if pain is severe. Nausea and vomiting are common; inform nurses if severe symptoms occur. Pain relief is usually by patient-controlled analgesia or epidural analgesia.
Wound care
- Wound is covered by sterile dressing after operation.
- Keep wound dressing dry; staples or clips will be removed on post operation day 7-14.
- Avoid kinking or knotting of surgical tubes such as naso-gastric tube, urinary catheters and intravenous catheters.
- Abdominal drain may be placed for removal of dirty fluid, and it is usually removed on day 2-5 depending on the content and volume of fluid drained.
Activity
Early ambulation and deep breathing exercise can help reduce the chance of chest infection or pulmonary embolism.
Diet
- Diet is restricted in the immediate postoperative period; it is gradually resumed (fluid, soft and normal diet) when bowel function returns.
- Bowel opening is loose and frequent in early period, but condition will improve with time.
-
Things to take note on discharge
Diet
There is no need to restrict diet; drink more water and take a high fibre diet to allow easy bowel opening.
Wound care
- Mild wound pain is common.
- Taking shower is allowed, but remember to keep dressing dry.
Activity
- Can resume normal daily activity within 1-2 weeks (according to individual situation).
- Avoid lifting heavy objects, bending or extending the body excessively in the first 4 weeks.
Follow up
- Remember the dates to remove the stitches or clips in the clinic.
- Follow up the clinic as scheduled for pathology result and assessment.
-
Remarks
For further information please contact your doctor.